My successful Home Birth after Caesarean - Rae
This is my story of how the birth of my second daughter Elsie, at home, turned out to be a wonderful, fulfilling experience.
Quite soon after I had an emergency caesarean with my first daughter Amelie, now aged 2, I began reading widely about having a vaginal birth after caesarean. I also met with a consultant to discuss why I had had an emergency caesarean and what this meant for any future pregnancies. During this process I became more and more convinced that the hospital experience during my first labour ultimately led me down a path that would result in an emergency caesarean. To this day I feel the caesarean was unnecessary and could have been avoided if I had had better midwifery support, been placed in a less clinical environment and if I had had the opportunity to have an active labour rather than being restricted to a bed, which slowed Amelie’s descent.
With my first pregnancy I was entering the world of the unknown and felt that having my baby in hospital was a ‘safe’ decision. My labour started on my due date with a few contractions in the early hours of Saturday. These contractions continued with long gaps in between until morning and were accompanied by a clearing out (a side effect of prostaglandins hormone release). By mid morning the contractions had passed and I went to lunch with a friend (spare underwear and leggings in a bag) and at around 5pm the contractions slowly began again, continuing all through the night and the next day until Sunday evening at 9pm when by then they were much stronger and every 4 minutes apart.
The pain was uncomfortable and building so we decided to call the hospital and, with a feeling of excitement and adrenalin, we were told to go in and I was found on arrival to be 2cm dilated.It was a quiet night so the midwife told us to stay to see how we progressed. About three hours later another labouring lady joined by her partner and mother-in-law were led into the waiting room (the room you are restricted to if there are no beds or, as in my case, not in ‘active’ labour). The lady was checked and told to go home as she was told she was neither dilated nor contracting, but she refused to leave: having had several children she knew her body and the signs. Sure enough, five minutes later after she had paced the corridor she let out a blood-curdling scream and fell to the floor. A team of midwives ran to her aid and announced that she was having a panic attack. It turns out, however that she was actually in labour, and shortly afterwards she gave she gave birth there on the bed next to my partner and me– much to everyone’s surprise, apart from her own.

Shortly after this I was examined and, not surprisingly, I was no longer dilated and was told to go home. ‘That’s what you just told her’, I thought. At 3am Monday morning, just back from the hospital and in my pyjamas, I laid down ready to sleep when my waters broke. Another call to the hospital and we were on our way back in. This time the contractions were a lot more painful and the car journey hellish, but again on arrival I was only a few centimetres dilated and so was made to wait in the holding room for another 11 hours whilst other labouring women came and went.
By this time I was on the gas and air and trawling a canister behind me whilst I tiptoed through the brand new ward (which was open but not in use due to low staffing) with every contraction trying to speed things up. On Monday at 2pm I started to panic, the midwife had been gone for hours, the pain started to feel different and I was scared the baby was coming. I begged my partner to get the midwife over and over again but he was told she was covering someone else’s shift. When she finally arrived she did a vaginal examination and exclaimed in a very impatient tone ‘you are ONLY 4 cm’.
How could I go on if I was only 4 cm, I thought? I had been at this for three days and my energy, my willingness, my strength and trust in my body had shattered. My mum, upset at seeing me in distress, had been encouraging about an epidural and at that moment I thought why not? If only I had read more and realised this would increase my chances of having a c section. When I asked the midwife for an epidural she rolled her eyes and I was finally taken to my own room.Once I was in a private space and at the thought of some pain relief I remember feeling like I could actually manage the pain. As the surgeon put in the tube I thought ‘why am I having this? I feel in control now.’ A doctor was in the room at this point and I remember him asking the midwife why I was having an epidural? She rolled her eyes again and he tutted, both now with their backs to me. I wondered why I was experiencing this negativity? If the doctor and midwife thought it was a bad idea, why didn’t they say something or offer another form of pain relief first - such as positivity and encouragement?
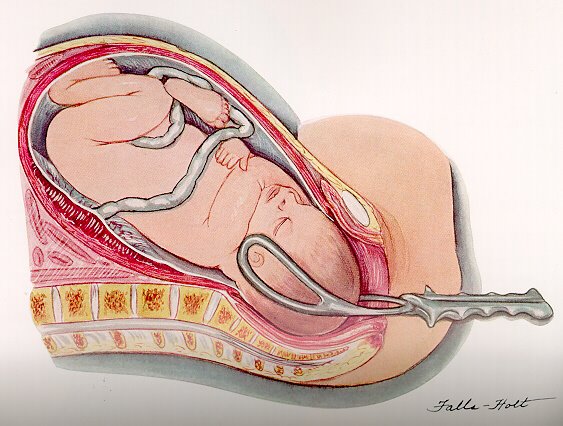
Now I was stuck on the bed (and so, not able to have an active labour) with a foetal monitor clipped to my baby’s scalp which, we found afterwards, had led her to bleed and bruise. The machine beeped away and every time it changed slightly my partners stress levels would peak and the midwife would jolt. At 9pm on Monday I was found to be 10cm and the epidural was starting to wear off. I didn’t want a top up so that I could feel to push but the midwife asked me ‘what was the point of having one?’ and promptly administered some more of the drug. In that brief moment before the top up I had begun to feel a strong urge to push but the midwifes were changing over and I was not allowed to do anything until she read through all my notes.
Finally at 10pm I was told to push,which I did for a few contractions, then I was told to stop, as I was to have an episiotomy rather than tear followed by a ventouse. Had I known that tearing naturally heals better, bleeds less and is less likely to get infected I would have refused the episiotomy. We tried another three times with my legs stuck in stirrups but to no avail. By this point I was delirious having not slept in three nights and everything started to become a blur. Paperwork was shoved at me to sign and I was whisked into surgery for failure to progress. My baby was born at 1am on Tuesday morning with a good APGAR score (the test used to quickly evaluate a newborn's physical condition and to determine any immediate need for extra medical or emergency care), though it felt like forever until her first cry. I didn’t get to hold or see her for another 30 minutes, no skin to skin, and she was sent away with dad whilst I was stitched up. When I finally had my baby in my arms and happily latched on to my breast my partner was told to leave. I was exhausted and couldn’t keep my eyes open, falling asleep with baby in arms and with no one to help.
That first night in hospital was terrible - my daughter screamed and screamed and I kept trying to feed her but after labouring for three days I would pass out only to be woken by a midwife shaking my arm. I really needed more support but my partner wasn’t allowed in and the hospital couldn’t provide it.
Four days after the labour and still at the hospital I was so annoyed and frustrated by the lack of help, given that I had just had major surgery and was expected to lift a baby on my own, that I tried to discharge myself, but I was told that I was supposed to have an iron test but no one had got round to doing it. So, as it turned out, with seriously low iron levels I left and for at least 6 months afterwards would find myself crying to sleep feeling that I had failed my little girl.
A year later I was pregnant again leaving a 20-month gap between my first and second child and, as far as the obstetricians that I met were concerned, not a large enough gap for a successful vaginal birth after caesarean.
Having done my research I let the obstetrician know at my twelve-week scan that I wanted a home birth after caesarean. The OB refused to support my decision and called in her manager to reiterate the risks (risks on which I was already self-informed). Her manager stated that I would have to have my baby in hospital as that’s where the doctors and midwifes ‘felt happiest’. When I responded that I would not be happy or calm in hospital, he retorted ‘that’s the theatre of life, darling’!
Disgusted by this attitude I immediately transferred from that well-respected central London hospital (who also wouldn’t allow me to use the birthing centre should I get moved to the labour ward as it would affect their end of year statistics) and I went back to my local east London hospital, where they did support my HBAC decision.
Despite this new-found support I never actually felt supported – I was called to several meetings with obstetricians where I was quizzed about my reasons for wanting a HBAC even though I had gone through the notes from my first labour with them and they saw no reason for it not to be a successful vaginal delivery. They questioned whether I was I just being obstinate with regards to my first labour as procedures had apparently improved, and they asked what made me think I could labour naturally anyway? And then came the risks, which are centred on uterine rupture, and I was faced with comments like ‘you are risking fatality of you or your baby and you could lose your womb’.
I wasn’t being obstinate, I had done my research on uterine rupture, I understood the risks and had gone through my the notes from my first labour with a specialist who agreed there was no reason why I shouldn’t be able to labour naturally. If at any point the conditions of my pregnancy had changed to further complicate things I would have re-evaluated my position.
With all this negativity I focused on keeping well informed and stood my ground with consultants, doctors and midwives. I made sure that I had a plan B birthing plan should I not be able to give birth at home. I also had the support and expertise of a wonderful Doula, Marcia, who had been through four very different births of her own.
Throughout the pregnancy I felt very isolated and found myself reading others’ VBAC and HBAC birthing stories online when I came across the Hackney home birth support group which meets monthly to share information, advice and stories. At this get together I met a midwife from the Homebirth team who immediately stood out as highly competent and unfazed by my HBAC decision. I called the Homerton home birth team leader days later and requested this midwife, as I wanted to ensure that I had someone with the right attitude to support my pregnancy and labour.
At 37 weeks pregnant I began to have regular cramps, which woke me up at night and eased off when I tried out different positions. I prepared for an early labour as my first labour started on my due date. I packed my hospital bag just in case, borrowed and tested a birthing pool, continued to listen to my hypnobirthing CD regularly and laminated my birthing plan. However, my due date came and went, - the cramps increased but by then I ignored them and tried to continue as normal.
At 40 + 4 weeks my midwife called me to say that the hospital were concerned and that if I had not had my baby by the end of the week I would need to meet with the obstetrician who would want me to have a caesarean. I felt sick at this news and considered having a membrane sweep despite not wanting any intervention.
A day later I spent the evening having contractions every ten minutes but by midnight they had stopped. I knew it wouldn’t be long and sure enough the next evening, 15 minutes after I had said goodbye to a friend who had come for dinner, I had a contraction which led me to the bath and my partner started timing. Minutes later at 10.15 my waters popped and immediately I was in immense pain, jumping out of the bath and on to the toilet to flush my system.The contractions went from 5 minutes apart to 3 minutes apart within 30 minutes and the need to bear down was uncontrollable. The midwives and my doula arrived about an hour and a fifteen minutes later, much to the relief of my partner, and I moved to the bedroom floor with no time to set up the birthing pool (not that I wanted it as I had briefly got back in the bath and it had made me feel sick. I preferred the cold water my partner squeezed over my head).
My doula and the midwives aided in keeping me active - moving me from all fours to a squatting position, helping the baby to descend. In fact the baby was descending so fast that my midwife found it difficult to read the baby’s heartbeat, which was causing concern. However, any concern she had was not shown to me, which I appreciated.
Close to the end with more failed attempts at foetal monitoring the midwife turned to me and said ‘let’s get this baby out’ and that’s exactly what I did, squatting, held by my husband and screaming at the point of ‘ring of fire’.Baby Elsie was born weighing 8lb 6, at 1.17am, three hours after labour had started.
At no point did I feel even a twinge at the site of my caesarean scar. So, after much unfounded stress, I got everything I wanted: no intervention, pain relief or vaginal exams. My placenta came naturally 30 minutes later and it all ended with a nice shower and a cup of tea. Despite plans to send my daughter to her Nan's when I went into labour we didn’t even have time to call until after the birth and she slept soundly through it all, waking up the next morning to her new sister.
It was amazing and very fast compared to my first labour and excitingly I got to see the baby slowly descending and crowning in the bedroom mirror which just happened to be opposite. Seeing her head slowly emerge helped me get through those final moments.
If I could offer any advice to anyone considering a HBAC it would be to keep an open mind, do your research, keep informed and be prepared for things to change. Keep communicating with the doctors and obstetricians despite the frustration you may feel at hearing ‘the risks’ for the tenth time. It was really helpful for me to understand the situation that led to my caesarean and from that to build confidence in my body and its ability to labour naturally.
One of the wonderful perks of having the home birth was that I really got to know my midwife and, unlike in a busy hospital environment, my midwife would stay with me during the labour rather than disappearing for hours covering more than one birth.
My final piece of advice would be to make sure you get the right support. At one point I had a midwife that grunted at me when I mentioned birthing in a pool and was forceful about giving vaginal exams. I changed midwifes and it immediately relieved the stress and got me what I wanted.
I know the struggle and the feeling of isolation at times in the fight for a HBAC so if anyone wants to email me for a chat please do raebow49@hotmail.com